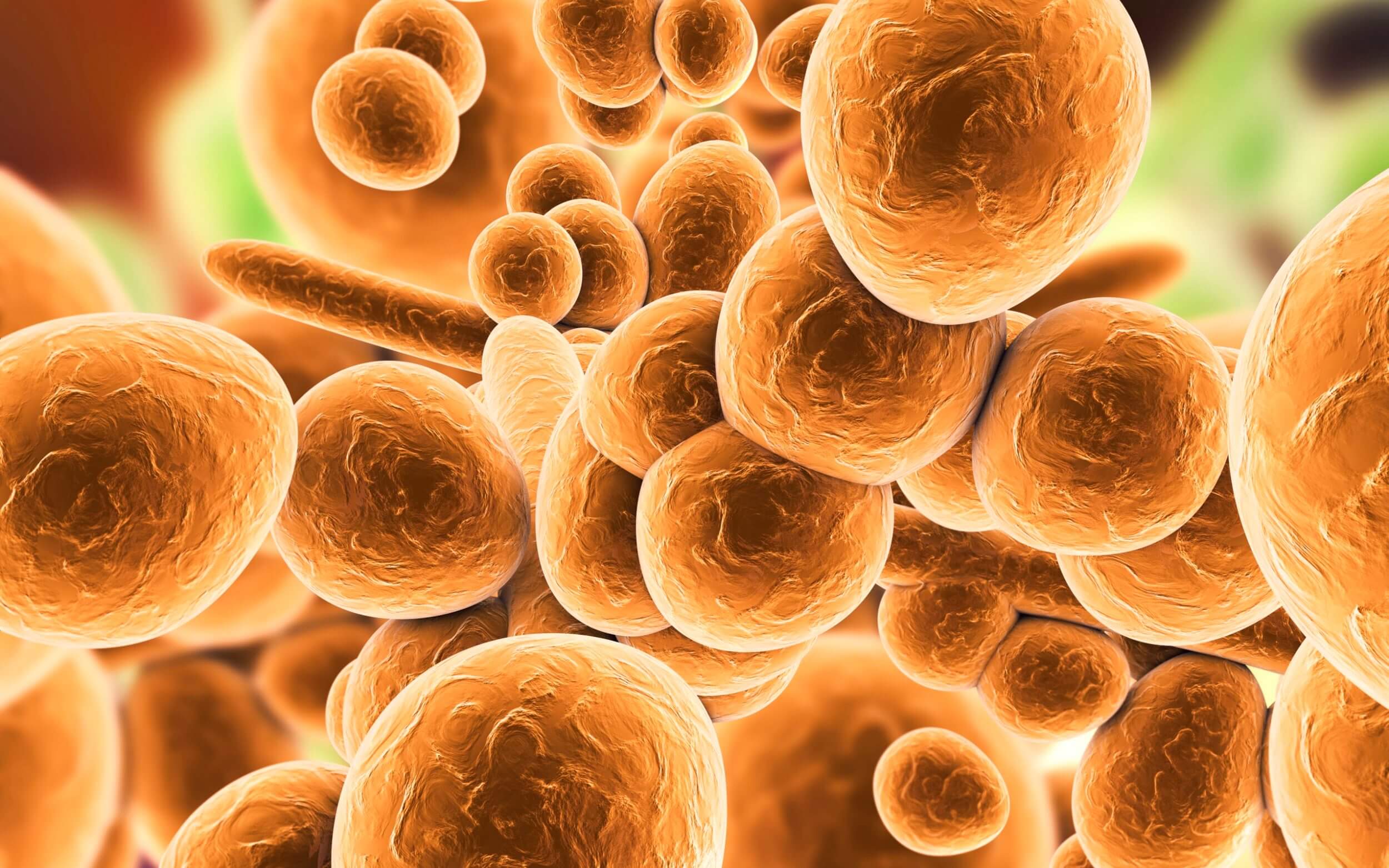
Expert warning as deadly drug-resistant fungus hits 36th US state – after cases shoot up 95 percent in two years
A rare and dangerous fungus that can cause severe infections and even death has been spreading rapidly across the US, according to a new report from the Centers for Disease Control and Prevention (CDC).
The fungus, called Candida auris or C. auris, is a type of yeast that is resistant to most antifungal drugs. It can contaminate medical equipment and surfaces in hospitals and other health care facilities, and then infect patients with weakened immune systems, such as those with cancer, diabetes, or organ transplants. The infection can affect various parts of the body, including the bloodstream, the brain, and the heart, and can lead to sepsis, a life-threatening condition.
The CDC has been tracking C. auris cases since 2016, when it was first reported in the US. Since then, the number of cases has increased dramatically, especially in the last two years. The report, published in the Annals of Internal Medicine, found that the number of infections rose by 59% from 2019 to 2020, and by another 95% from 2020 to 2021. By the end of 2021, there were 1,471 confirmed or probable cases of C. auris in 36 states.
The report also found that the number of people who were colonized by C. auris, meaning they carried the fungus on their skin or in their body without showing any symptoms, also increased significantly. The number of colonized people rose by 21% from 2019 to 2020, and by 209% from 2020 to 2021. By the end of 2021, there were 4,041 colonized people in 29 states.
The CDC warned that C. auris poses a serious threat to public health, as it is difficult to identify, treat, and prevent. The fungus can be easily misdiagnosed as other types of Candida, which can lead to inappropriate or ineffective treatment. The fungus can also persist on surfaces and equipment for long periods of time, and can spread from person to person through contact or through the air. The CDC recommended that health care facilities implement strict infection control measures, such as wearing gloves and gowns, cleaning and disinfecting the environment, and screening and isolating patients who may have C. auris.
The CDC also urged health care providers and laboratories to report any suspected or confirmed cases of C. auris to their local or state health departments, and to send samples to the CDC for further testing and surveillance. The CDC said that early detection and timely response are crucial to contain the spread of the fungus and protect patients and health care workers.
The CDC also advised the public to be aware of the signs and symptoms of C. auris infection, and to seek medical attention if they develop any of them. The symptoms may vary depending on the part of the body that is affected, but they may include fever, chills, fatigue, pain, redness, swelling, or discharge. The CDC said that people who have recently been hospitalized, have received antibiotics or antifungals, or have underlying health conditions are at higher risk of getting C. auris infection.
C. auris is not the only drug-resistant fungus that has been causing concern in the US. In December, the CDC reported an outbreak of a different type of Candida, called Candida glabrata, that was resistant to all three classes of antifungal drugs. The outbreak occurred in a long-term care facility in Washington, DC, and affected 101 residents and 22 staff members. Eight of the residents died from the infection.
The emergence and spread of these drug-resistant fungi highlight the need for more research and development of new antifungal drugs, as well as better stewardship and surveillance of existing drugs. The CDC said that it is working with partners to monitor and respond to these fungal threats, and to prevent further resistance and transmission.